List of services offered
Family dentistry
Our family dentistry service allows us to meet the specific needs of all family members, from the youngest to the oldest! Identifying problems early and taking care of them helps them maintain their oral health for life.
Our three (3) major goals in family dentistry
1 | Provide dental care tailored to the needs of the whole family. It starts with the little ones…
We attach great importance to the care of children. The atmosphere is always relaxed and fun to build trust. We want every visit to be a positive experience.
Our priority is to ensure the normal growth of primary teeth, as they play a key role in chewing, language development and the appearance of permanent teeth. The first visit is from the age of 2, but can be done earlier if necessary.
Essential oral care:
- Check the condition of the teeth;
- Check the position of teeth and tongue when swallowing;
- Screen for speech and chewing problems;
- Detect and treat cavities early;
- Respond to parents' concerns about any stains on the teeth, discomfort, injury or swelling of the gums.
Monitoring tooth growth:
- Check the progress of jaw growth;
- Ensure adequate growth of primary teeth in terms of sequence of appearance and alignment.
2 | Offer a preventive approach in orthodontics
The preventive approach in orthodontics aims to detect problems early and apply solutions without delay. This prevents the development of complications that may require extractions, surgeries or more extensive treatments later. While the primary teeth are still present and the growth is not complete, it is possible to detect skeletal problems in the mouth. When necessary, a first step of orthodontic treatment can begin.
The expansion of the palate performed at an early age gives more width to the upper jaw. This has the effect of allowing better alignment of the permanent teeth and creating a better occlusion.
3 | Offer an educational component
It is also important for us to have an educational approach. We help children in their learning and support their parents so that they are comfortable in their role of supporting dental care. Likewise, we suggest solutions to make brushing accepted or to help little ones to put on their orthodontic appliance.
The preventive measures and advice aim to:
- Develop healthy eating habits;
- Adopt good oral hygiene practices and good brushing technique;
- Encourage periodic visits to the dentist;
- Promote the importance of regular cleaning by the dental hygienist;
- Offer preventive treatments, such as the application of dental sealants that offer protection against cavities.
Our mission is to help children keep their mouths healthy, but also to become adults who are aware, responsible and autonomous when it comes to their oral health.

Technologies
Technologies are valuable allies for your oral health. Here are some of the cutting edge instruments that you will find at the Dr. Susan Biner Dental Clinic. These facilitate the rapid detection of diseases, the establishment of an accurate diagnosis and the effectiveness of treatments, directly improving the oral health of patients.
TRIOS®
The TRIOS® intraoral scanner provides fast and comfortable optical impression taking in addition to enabling the design and fabrication of computer-assisted restorations.
Not only does this technology generate high-resolution color images, it also produces ultra-precise ceramic restorations.
Crown
It repairs and strengthens a very damaged, heavily decayed tooth or one that has undergone root canal treatment. It completely covers the tooth, which gives it back its aesthetics, its function and its initial solidity.
Veneer
It is a thin ceramic shell, bonded to the front surface of the tooth, which is used to correct a minor cosmetic defect. It is strong and perfectly reproduces the appearance of a natural tooth.
Overlay
It is a custom-cut ceramic block inserted into a tooth in place of an old broken restoration. It is also used to repair major decay that can weaken the tooth. The encrustation firmly repairs the tooth and gives it greater resistance.
Benefits
The scanning speed and the quality of the images make the procedure much more comfortable. The diagnoses are more precise and more sophisticated treatment protocols limit the time spent in the chair. The patient experience is therefore greatly improved. This innovative technology produces high-precision restorations that require little or no adjustment. You will thus obtain a functional, solid, durable and natural-looking restoration in time!
CariVu®
CariVu® is a small, compact and portable device that detects cavities. The tool is positioned on each side of the tooth and sends it an infrared light at a very short distance which illuminates it completely. The precise images read like an x-ray. The enamel becomes transparent, but any carious lesion remains dark. By seeing through the tooth, the dentist can easily detect abnormalities and cavities at a very early stage.
It can provide a second opinion on the x-ray to confirm a diagnosis and help make decisions about what treatment to do.
DIAGNOdent®
The DIAGNOdent® device is a diagnostic tool that lends a hand to other traditional methods (visual examination, radiography, explorer (dentist's hook). This device uses a fluorescence laser which detects the onset of caries very early. He can see what is still too small to be seen by other methods and measures the degree of demineralization of the tooth, revealing bacterial activity.
Its small size allows it to access hard-to-reach areas, right down to the bottom of the dental arch. Its use is fast, safe and painless. Taken at an early stage, decay requires only minor restoration. This has the advantage of being done without anesthesia and of being more durable.
VELscope®
VELscope® technology is a revolutionary system that enables the early detection of oral cancer. Since 80-90% of oral cancers can be cured if detected and treated quickly, the VELscope® is a particularly valuable tool.
This device helps the dentist to examine the lining inside the mouth, looking for abnormal lesions and precancerous cells. Lightweight and portable, it projects fluorescent blue light. Healthy cells reflect light, while a dark mass reveals the presence of abnormal tissue or cancer. A few minutes are enough to carry out such an examination.
Digital radiography
Digital x-rays are used to look at the teeth, gums and bones that make up the oral cavity. Generating considerably less radiation than traditional film photographs (which emit very little radiation), this device is safe and comfortable. Its versatility allows you to take a variety of photos, including panoramic (Panorex), bitewing x-rays and cephalograms.
The precision of the images it produces makes it an indispensable diagnostic tool in order to more easily detect oral abnormalities at an early stage. As the images are digitized, they are easily transmitted to another healthcare professional and are archived in the electronic patient record for future reference.
Device to treat Obstructive Sleep Apnea (OSA) and snoring
Sleep apnea is an often unrecognized and yet very common condition. It is a sleep disorder that interrupts breathing. Most people don't know they have OSA (obstructive sleep apnea) and therefore go untreated.
At the Dr. Susan Biner Dental Clinic, we can make mandibular advancement braces to control sleep apnea or snoring.
To make these devices requires extensive training in sleep medicine. Dr Biner graduated from the American Academy of Dental Sleep Medicine (AADSM) with a Mastery 1, 2 and 3.
Learn more about sleep apnea
Teeth Whitening
The different ways to whiten teeth
- Teeth whitening at home using custom trays.
- Whitening at the dentist's chair.
- Use of over-the-counter bleaching products.
 Teeth whitening products, whether over the counter or professional in-clinic treatments, use hydrogen peroxide. This ingredient effectively removes stubborn stains from the surface of the teeth.
Teeth whitening products, whether over the counter or professional in-clinic treatments, use hydrogen peroxide. This ingredient effectively removes stubborn stains from the surface of the teeth.
It should be noted, however, that the concentration of whitening product, and therefore the quality of the results, varies greatly depending on the nature of the treatment. In fact, over-the-counter products contain a minimal concentration of peroxide, while professional products used during treatments offered by the dentist have a much higher concentration.
Contraindications
- Pregnant or breastfeeding women.
- Person with Crohn's disease (ulcerative colitis).
- Person with chronic heartburn.
- No one, so the immune system is weakened by cancer, AIDS, an autoimmune disease, etc.
- Person with significant problems in the temporomandibular joint (TMJ) or bruxism.
- Person who wears braces.
- Cavities and gum disease.
It is important that teeth whitening is done under the supervision of your dentist. It is by doing a dental examination that the dentist can diagnose the cause of the discoloration, to estimate the duration of the treatment and what the chances of success will be. As for the final result, it remains difficult to predict, and no guarantee can be given.
Possible side affects
- Tooth hypersensitivity | This sensitivity is usually transient and disappears when treatment is stopped. If this sensitivity occurs during treatment, stop treatment and consult your dentist. Your doctor can prescribe a desensitizing toothpaste that you can place in your tray for 30 minutes for a few days to eliminate sensitivity.
- Gum irritation | Gum sensitivity can be the result of an ill-fitting trays or it could also be that you place too much gel inside the aligner and the overflow of the product irritates your gums to the point of developing small ulcers. In either case, you should stop the treatment and consult your dentist.
- Throat irritation | Too much gel can cause the product to overflow. This irritation is short-lived, as long as you are warned to spit and not swallow the excess gel.
- Discomfort in the joint | This sensation occurs especially when you wear the aligner because your teeth no longer close exactly together.
How long do teeth stay white after treatment?
It varies a lot from one patient to another and according to each patient's habits. For most people, the effect persists for a period of two to five years. This is why we recommend a treatment of a few days 1X per year to maintain the desired whiteness, FOR LIFE.
SEE LIFETIME WHITENING – Offered to all our regular patients.
 Teeth whitening at home using well-adapted trays
Teeth whitening at home using well-adapted trays
At-home teeth whitening is a do-it-yourself solution, offered at a lower cost than chair-based teeth whitening. What is advantageous and appreciated by patients, what is possible to do the treatment in the comfort of the home, at the time chosen by the patient.
Most patients notice a difference within 10 to 14 days, and the full results appear at the end of the treatment period. This type of treatment is based on the use of personalized trays, made from impressions of the teeth. This ensures an even application of the product during processing.
The procedure
- During a first appointment, the impressions are taken so that the trays can be made in the laboratory.
- During a second visit, the aligners are given to the patient, and he receives instructions from the dental team.
- At the right time, the patient applies the right amount of gel to their trays and places it on their teeth. They must remain there for a predetermined period.
- The last step is repeated every day, for the entire duration of the treatment.
- An appointment is scheduled at the end of the treatment to assess the results.
Recommendations for use when whitening at home
- Do not smoke when using the bleach.
- Do not eat or drink with the trays in your mouth.
- Clean and store gutters thoroughly.
- Keep the bleach away from heat. Syringes that are not can be placed in the refrigerator.
- Avoid drinking soft drinks, grape juice, red wine, tea or coffee to avoid staining the teeth.
- For best results, don't skip a day.
- Make 10 to 14 applications.
 Application procedure
Application procedure
1 — Brush and floss your teeth well before proceeding with the treatment.
2 — Apply a thin layer of gel along the front base of the trays.
3 — Insert the trays into your mouth and sit them firmly.
4 — Wipe off excess with your finger.
5 — Keep in the mouth for 30 minutes during the day or all night (depending on the treatment chosen). When the treatment is complete, rinse or brush your teeth and trays.
Whitening in the chair
Chair whitening is the fastest teeth whitening method currently available. Since its results are immediate, this procedure is ideal for people who want to improve their appearance very quickly for a special occasion such as: a wedding, a conference, a television interview, etc.
 The procedure
The procedure
Since in-office whitening is performed by a qualified dental professional, it is also a safe and reliable procedure. Dentists do not offer whitening to patients who do not have an oral health exam beforehand. Indeed, such an examination is always necessary to determine the cause of the yellowing of the teeth, as well as the feasibility of a whitening treatment.
Chair whitening occurs as follows:
1 — The gums and soft tissues of the mouth are protected to prevent the whitening product from coming into contact with them.
2 — The whitening gel is applied evenly to the teeth.
3 — The gel is activated with a special light, which whitens the smile by removing stains.
You can repeat the last steps a few times, until you get the bright smile you want. The whole process usually takes between 60 and 90 minutes for a full mouth. In some cases, two appointments may be necessary to achieve the desired whiteness.
Once the treatment is complete, you will immediately see the difference!
The results
The chair teeth whitening technique is very effective and can achieve up to 8 shades more discoloration. After your treatment, your teeth will be considerably whiter. However, the degree of whitening depends on the starting color and the type of teeth you have.
Generally, people with yellow-colored teeth will get better results than those with white, brown, or gray teeth. You can expect the results to last between 1 and 3 years. Your diet, the medications you take, and smoking have an influence on this time.
The cost
We often have promotions for this type of laundering. Check our site frequently for the best discounts. Our price for armchair whitening always includes a whitening kit to take with you with your own custom-made trays. This whitening kit to take with you will keep your beautiful white smile for a long time.
Dental sealants
Dental sealants are a preventative measure. They can prevent cavities from forming in the grooves of permanent premolar and molar teeth.
What are pits and cracks?
Pits and fissures are deep furrows, crevices or natural cavities found mostly on the chewing surface of permanent molars. The toothbrush can hardly remove bacteria and food debris that lodge in it. Studies show that fluorides are also ineffective in this condition. This is why a high number of dental caries is attributable to pits and fissures.
About 80% of cavities are found on teeth that have deep furrows since they are more difficult to clean with a toothbrush.
Dental sealants are highly recommended for children, adolescents and even adults. There is no age when it comes to protecting your teeth from decay. (Especially when the molars and premolars have deep grooves) Our very acidic diet and the amounts of added sugars put us all at risk of cavities. Sugary drinks, coffee, alcoholic beverages, and lots of snacks are the worst for your teeth. The lack of saliva with the many drugs that we take, the loosening of the roots that occur with age and suboptimal hygienic techniques are situations at high risk of cavities.
The furrows are, most of the time, very fine, to the point that the bristles of the toothbrush cannot get rid of all the food residues after the meal. To overcome this inconvenience, the dental professional applies sealant, which fills the grooves and helps to level the occlusal surface and prevent fine particles from seeping into the interior of the tooth.

Benefits of dental sealants
- The dental sealant is an aesthetic option, white in color and practically invisible in the mouth;
- Once installed, the sealant lasts for several years (between 3 and 10 years);
- This procedure is very simple, fast and economical;
- No local anesthesia is necessary;
- This is a 100% painless technique.
- Economic | The application of sealant represents on average half to one third of the cost of making a filling to treat cavities.
What are the main steps in effectively applying dental pit and fissure sealant?
Usually made from resin and glass ionomer cement, dental sealant sets in very quickly. It only takes one appointment to benefit. Afterwards, brushing your teeth becomes much easier since the surface will be more flat.
There are a few steps you need to take to apply dental sealants. Nevertheless, these are simple, painless and harmless to the patient.
- The dentist first performs a careful examination of the patient's teeth and condition to determine the appropriateness of applying dental sealants;
- The teeth that will receive the sealants are cleaned. A solution is then applied to promote the adhesion of the sealants to the teeth;
- The teeth are then rinsed and dried;
- The sealants are applied to the teeth to be treated, then they are exposed to a special light which will allow the material to solidify.
Once these steps are finalized, you can count on an unparalleled protective barrier for your oral health. Of course, follow-up visits can be made and good brushing habits are also a must.
Act quickly to increase the effectiveness of the treatment
It is always easier to prevent tooth decay when adult molars are erupting. Once they have come out completely, the dentist is able to detect pits and cracks during a routine examination. If there is a lot of dental plaque, it becomes especially important to see a doctor before the buildup decays your tooth.
Acting between the ages of 6 and 14, as adult teeth develop, is the best way to prevent such inconvenience. However, when the dentist deems it necessary, the dental sealant can also be used in adults at risk of developing cavities.
In conclusion, although dental sealant is an option to improve your child's dental health, it is important to keep in mind that its application does not replace regular dental visits.
Consulting a dental health professional allows you to smile to the fullest, without any cavities or bite problems. Aesthetic, simple, painless and inexpensive, dental pit and fissure sealer is the easiest way to protect your teeth or those of your child.
Early detection of cavities | DIAGNODent®
A cavity is an infection that attacks the hard tissue of a tooth. First, the cavity forms on the outermost layer of the tooth (i.e., the enamel), then it progresses toward the centre of the tooth (i.e., the dentine). Eventually, it can reach the pulp, which contains the nerve and blood vessels.
Cavities are caused by bacteria found in plaque.
Dental check-up
Cavities are often detected during a dental check-up. The dentist uses tools to assess the condition of your teeth and look for any cavities.
Traditional methods to detect cavities include :
- Visual examination, with or without a magnifying glass
- Dental explorer
- X-rays
Unfortunately, these methods can’t detect all cavities. In fact, all of these methods combined only allow a dentist to detect 49% of cavities. Despite their skills and the tools at their disposal, dentists know that half of the dental cavities go undetected during a check-up.
Why such a low detection rate?
The pits and fissures on the surface of teeth are often quite narrow, making it difficult for the explorer to reach deep enough to detect a cavity. In other cases, a cavity can form under the tooth’s surface, making it even harder to detect. And, at a very early stage, cavities are very small and difficult to see.
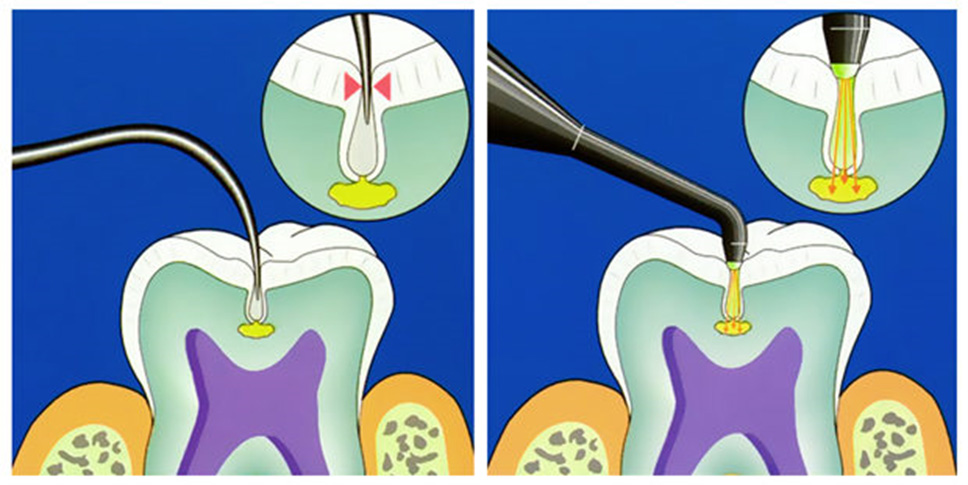
DIAGNODent® | For an exceptionally precise diagnosis
DIAGNOdent® is a state-of-the-art technology that is revolutionizing how dentists detect cavities. Its 90% cavity detection success rate is significantly higher than traditional methods.
DIAGNOdent® uses a fluorescent laser to measure a tooth’s level of demineralization and detect bacterial activity. This extremely precise diagnostic tool instantaneously transmits the information it collects to the dentist. Any anomalies are translated into sound and visual signals.
The DIAGNOdent® tool is perfectly safe and painless because it does not come in contact with teeth. The laser “sees” what traditional methods miss. The tool is about the size of a crayon and can easily access hard-to-reach areas, like the pits and fissures in molars. DIAGNOdent® makes it possible to do an in-depth check-up of your teeth.
Advantages of laser detection :
- Easy and comfortable to use
- Safe and painless
- Precise and fast
The importance of early detection
Since cavities can progress quickly, detecting them early is important. In its early stages, a cavity is easy to treat. Minor restorations are much more durable and can be done without the use of anaesthetic. If left untreated, a cavity can cause intense pain and require a root canal, which is a much more complex procedure. In severe cases, the tooth may even need to be extracted.

DIAGNOdent® provides a precise diagnosis, making the dentist’s work easier. However, despite its excellent performance, it cannot replace traditional diagnostic methods. This tool is used in combination with other methods to detect cavities early and precisely. This combined approach makes quick interventions possible, helping you maintain healthy teeth for longer.
Cavities
What is a cavity?
A cavity is a disease that affects the soft tissue of a tooth. It first attacks the enamel, then moves inward to the dentin and pulp, where the nerve and blood vessels are found. Since cavities don’t heal on their own, they must be removed with a dental treatment.
How does a cavity develop?
Bacteria cause cavities. They feed off of food particles left on teeth and spread to form plaque. When teeth aren’t brushed after a meal, this sticky, transparent film gradually thickens, forming a hard deposit called tartar, which can only be removed by a professional. Bacteria digest sugars, producing an acid that demineralizes tooth enamel, leading to the formation of cavities.
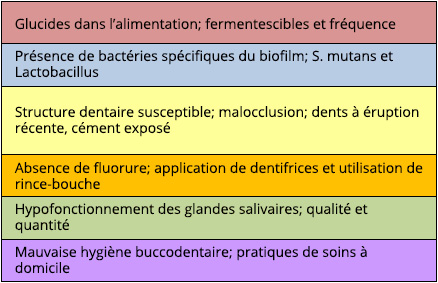
The table below is a guide for assessing risk factors for dental caries in a patient.
Our saliva possesses enamel-protecting properties and can:
- Help neutralize acidity
- Replace some minerals
- Wash away some bacteria to prevent plaque
Unfortunately, the power of our saliva is limited. If you eat too many sweets and snacks, your teeth are subjected to a larger amount of bacteria, which speeds up the development of plaque and tartar. With your teeth in constant contact with acidity, cavities are more likely to form.
Tips for stimulating the production of saliva:
- Eat a fruit
- Rinse your mouth with water
- Chew sugar-free gum that contains xylitol (a sugar substitute with antibacterial
properties)
Which factors lead to the development of cavities?
1 | Poor eating habits
Bacteria love sugary foods. Unfortunately, the acid produced when sugar breaks down can quickly demineralize tooth enamel. This is why a diet high in sugar is very damaging to your teeth. Limit your intake of the following foods :
- Candy, treats and gum that contain sugar
- Fruit juice, smoothies and flavored coffee
- Bread, pasta, cereal and prepared foods
The destructive effects of soft drinks, juices and energy drinks are a major cause of early childhood cavities as well as cavities in children and adolescents, especially among the low-income population and ethnic minorities. A 355 mL (12 ounce) soft drink contains 10 teaspoons of sugar as well as acids. Soft drinks and diet energy drinks contain citric acid and phosphoric acid, two substances that can directly lead to demineralization of the teeth. Rinsing your mouth with water, drinking through a straw, chewing gum containing xylitol, and consuming beverages that can cause cavities while eating can help reduce the negative effects of liquid fermentable carbohydrates.
For the same reason, the following acidic foods should be eaten in moderation:
- Citrus fruit and berries
- Wine and soft drinks
Be careful with sticky foods (dried fruit, caramels, gummies, etc.) that can adhere to teeth and are more difficult to remove.

2 | Poor oral hygiene
Poor oral hygiene often leads to cavities. For proper oral hygiene, do the following :
- Brush your teeth at least twice a day for two minutes
- Use dental floss before going to bed to get rid of any food particles stuck between your teeth
- Use fluoride toothpaste
- See your dentist once a year for a complete check-up and professional tartar removal
3 | Hard-to-reach areas
Some areas can be hard to reach when brushing. Because these areas are more prone to cavities, they warrant a little extra care. Pay special attention to :
- Grooves on the surface of teeth
- Interdental spaces
- Gum line
- Hidden surfaces due to tooth misalignment or overlapping
The importance of early detection
For best results, cavities should be treated as soon as they appear. In the first stage of a cavity, only the enamel is affected and no pain is felt. Only minor repairs are needed.
In the second stage, the cavity reaches the dentin, the softest part of a tooth. Patients may experience sensitivity to heat, no tooth pain. Repairs remain relatively minor.
Eventually, if left untreated, the cavity reaches the pulp, which is located in the center of the tooth. This causes sharp pain. A root canal, and possibly even an extraction, becomes inevitable. At this advanced stage, the infection can lead to an abscess, which causes sharp, throbbing pain.
Because cavities can progress quickly, it’s important to see your dentist regularly.
Cavity prevention
«There are a lot of benefits to identifying patients at high risk for cavities before cavities set in.»
— Institut National de la Santé (INS)
Many of our patients express concerns about cavities. Tooth decay remains the most common early childhood disease. But, fluoride isn't just for kids. Sufficient fluoride needs to be absorbed every day, regardless of our age, some adults are at higher risk, and should consume higher doses.
« To avoid cavities, it is important to get enough fluoride. »
— Association Dentaire Canadienne (ADC)
Here are some recommendations for you:
- Visit the dentist on a regular basis for professional tartar removal
- Maintain good oral hygiene
- Reinforce tooth enamel by using fluoride toothpaste
- Treatment with a fluoride varnish to recalcify the enamel every 6 to 12 months depending on your risk of cavities
- Putting dental sealants on teeth with a high level of decay
- Eat a balanced diet and limit your consumption of sugary and acidic foods
Follow these recommendations to stack the odds in your favor. You can prevent cavities and keep your teeth healthy for life!
Root canals | Endodontics
An infection that reaches the nerve of a tooth requires endodontic treatment, or root canal treatment. The dentists at the Dr. Susan Biner Dental Clinic allow you, by this solution, to keep your natural tooth instead of extracting it and to preserve the alignment of your other teeth. To complete the procedure, our oral health professionals recommend the creation of a crown to protect the tooth weakened by the root canal treatment and avoid any fractures.
What is root canal treatment?
It is an effective dental treatment that prevents the loss of natural teeth and thus prevents the need for implants or prostheses. Its success rate remains very high.
Why a root canal treatment?
- Damage to the dental pulp (nerve) by caries.
- A tooth fracture or crack that extends to the pulp.
- Trauma (stroke, stress, etc.) causing pulpal necrosis.
- If the survival prognosis of the tooth to be crowned is poor.
- Irreversible pulpitis (inflammation of the pulp, sharp pain).
When an endodontic lesion is visible on the root of the tooth.
Dental pulp is the part of the tooth that contains nerves and blood vessels. When it becomes infected, irritated or damaged, certain signs appear.
The symptoms indicating the presence of pulpal involvement are:
- Exaggerated sensitivity to cold and heat
- Tooth discoloration
- Swelling
- Gum pain
In addition, even if no symptoms are present or the prognosis for pulpal survival is guarded, root canal treatment may be necessary, simply to increase the success rate of future restorative treatments.
Root canal treatment
Root canal treatment involves devitalizing the tooth by removing the dental pulp and disinfecting the canals to allow the insertion of endodontic obturator material to the end of them.
The procedure
- The procedure begins with an x-ray in order to clearly visualize the shape and length of the canals to be treated. The treatment is then done under local anesthesia.
- Make the opening in the tooth to access the roots (The surgical field: (isolate the tooth using a rubber dam to prevent bacteria in your saliva from coming into contact with the tooth and ingestion of instruments used during treatment).
- Complete removal of infected pulp
- Cleaning of the channels in order to completely eliminate the bacteria present
- Hermetically sealing the cavity and canals with a waterproof material, so that no bacteria can infiltrate again
- Close the access cavity with a final restoration as soon as possible.
- The final restoration protects and restores normal function to the tooth. It could be a crown or, as the case may be, another type of restoration.
The tooth is devitalized, but the root canal treatment saved it.
Other very important points
Teeth with root canal treatment are not immune to decay or gum disease. Even dead, they will remain susceptible to erosion, attrition, abrasion, abfraction and decay.
If you maintain good dental hygiene and see your dentist regularly, your tooth could last as long as your other teeth.
A tooth that has had a root canal treatment becomes brittle and therefore more fragile, which increases the risk of dental fractures. In the majority of cases, it is advisable to restore such a tooth with a crown.
Root canal treatment may require 1 or 2 visits. After treatment, your tooth may remain sensitive for some time. If you experience severe pain or swelling, which is not common, see us as soon as possible.
Most of the time, a tooth that has had a root canal can be saved, but sometimes all attempts fail and there is no choice but to extract the tooth.
Why do we want to avoid tooth extraction?
Root canal treatment saves the natural tooth. When possible, keeping the dentition in place is the option recommended by dentists. A devitalized tooth can still play its masticatory role in addition to maintaining the balance and stability of the teeth. The natural tooth also supports the health of the jaw bone. It stimulates the tissues and muscles of the mouth and strengthens the bone structure. Maintaining the tooth prevents loss of bone mass.
Although endodontic treatment is a relatively common procedure, it's best to do your best to avoid it! Do not neglect to take care of a cavity. Diagnosed early, its treatment is much simpler. In addition, the dentist should be consulted promptly when a tooth becomes painful.

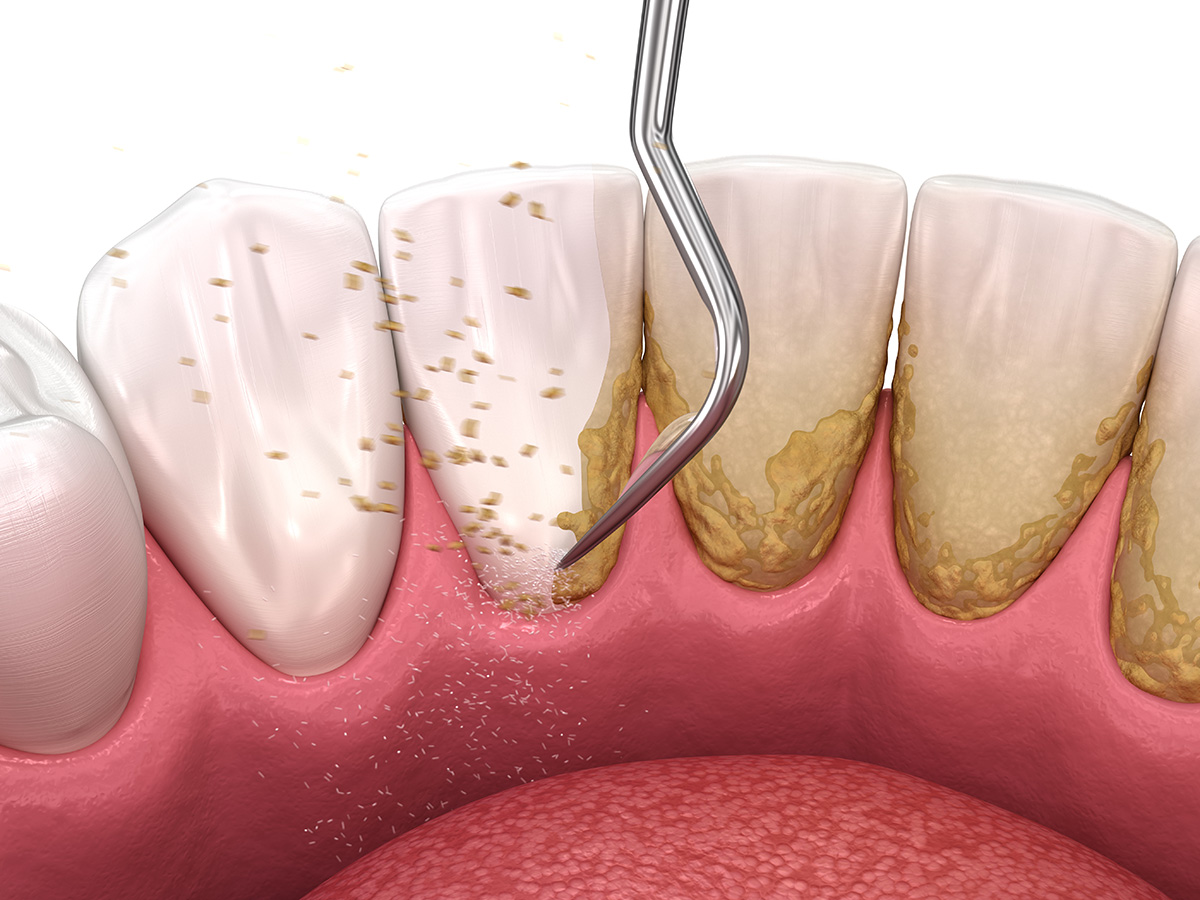
Gingivitis vs periodontitis
What is gingivitis?
Gingivitis is a benign infection of the gums caused by an accumulation of bacteria. Poor oral hygiene leads to the proliferation of this bacteria. A whitish film called plaque forms on the
surface of teeth and eventually makes its way under the gums, causing them to swell.
Gingivitis is a very common infection.
- Approximately 70% of adults will suffer from gingivitis in their lifetime
- 64% of pregnant women develop gingivitis
- 50% of people with diabetes suffer from periodontal disease
Signs of gingivitis
Because gingivitis is usually painless and subtle, it can sometimes go unnoticed.
Over time, the following signs may become more evident:
- Bleeding gums during brushing, flossing or eating (e.g. biting into an apple)
- Swollen, red gums
- Sensitive gums
- Bad breath
How is gingivitis treated?
Gum disease is treatable. First, a dental hygienist will remove all plaque and tartar from
your teeth. Then you must follow a rigorous oral hygiene routine that includes brushing twice a day and flossing before bed. This will stop gum disease from progressing and eliminate swelling.
Possible complication : Periodontitis
If nothing is done about gingivitis, it will worsen and, in 30% of cases, become periodontitis. This much more serious infection reaches the periodontium, which is all the tissues that support teeth (gums, cementum, alveolar bone, periodontal ligament).
Once affected by bacteria under the gums, the tissues can no longer carry out their functions, leading to serious oral health consequences.
In addition to gingivitis symptoms, periodontitis also leads to :
- Tooth sensitivity
- Gingival recession
- Loose teeth
- Abscesses
- In severe cases, loss of teeth
Treating periodontitis
Early intervention is best when treating periodontitis. It stops the illness from getting worse and restores the teeth’s support structures.
The periodontist prepares a treatment plan that can vary, depending on the severity of the situation :
- Deep cleaning of periodontal pockets to remove bacteria stuck on teeth and roots
- Surgery for severe cases
- Antibiotics to control harmful bacteria
- In some cases, gingivoplasty is needed to reshape gums, making them look more
natural and uniform around teeth
Prevention
To prevent gingivitis, plaque has to be removed from teeth every day. Naturally-occurring bacteria in the mouth has to be controlled and maintained at minimum levels to prevent them from insidiously attacking tooth enamel.
Proper oral hygiene is the key to success.
- Brush your teeth twice a day
- Use dental floss
- Use mouthwash
- Use the right toothbrush (small head and soft bristles)
- Use fluoride toothpaste
Practicing good oral hygiene is essential to gum health. Scheduling regular cleanings by a dental hygienist is also an important preventive measure.
Only your dentist can diagnose periodontal disease. Regular check-ups will help you maintain optimal gum health.

Treating periodontitis
What is periodontics?
Periodontics is a specialized branch of dental medicine concerned with periodontal health. It aims at assessing and caring for the periodontium, which is composed of the tissues that support teeth.
The periodontium includes :
The gums
Soft tissue that surrounds teeth and covers the jawbone. Their role is to support teeth and keep them solidly in place.
The alveolar bone
Part of the jawbone that contains the dental roots.
The cementum
Protects and completely covers the dental roots inside the alveolar bone.
The periodontal ligament
Located between the cementum and the alveolar bone. The tissue completely surrounds dental roots.
The nerves and blood vessels
Located in the centre of the dental root, as well as around the tooth in different areas of the periodontium.
What is periodontal disease?
Periodontal disease affects the various components of the periodontium. The most common periodontal diseases are gingivitis and periodontitis.
These diseases develop from bacterial and parasitic infections. Poor oral hygiene leads to an accumulation of bacteria on teeth, forming a sticky, transparent film called plaque. Plaque sticks to difficult-to-reach areas, between teeth and along the periodontal zone. If it isn’t removed on a daily basis, plaque calcifies and hardens, becoming tartar. The acid attacks the enamel, forming a cavity and causing swelling of the gums, or gingivitis. When gingivitis is left untreated, it can lead to periodontitis.
Risk factors
- Poor oral hygiene
- Diabetes
- Smoking
- Pregnancy or menopause (hormonal changes)
- Weak immune system (HIV, AIDS, leukemia, etc.)
Understanding gingivitis
Gingivitis is the first stage of periodontal disease. It is a common, minor inflammation of the gums. 70% of the population will suffer from gingivitis at one point, as well as 64% of pregnant women.
Gingivitis is caused by poor oral hygiene because bacteria proliferate along the gum line.
Symptoms
Since gingivitis is often painless, many people don’t know they have it until the following symptoms appear :
- Bleeding during brushing or flossing
- Red and swollen gums
- Sensitivity to heat
- Persistent bad breath
Treatment
- Professional tartar removal by a dental hygienist
- Brushing twice a day
- Flossing every night before bed
- Using fluoride toothpaste
To treat gingivitis, the dental hygienist will perform a deep cleaning of the teeth. Using various tools, the hygienist removes tartar accumulated along the gum line.
Good oral hygiene must then be practiced at home. Once the tartar has been removed and proper oral hygiene is maintained, gums can return to normal. The symptoms of gingivitis (redness, bleeding, etc.) will progressively disappear.
Understanding periodontitis
Periodontitis is the advanced stage of periodontal disease and the result of untreated gingivitis. Bacteria, which have infiltrated the gums, now infect the periodontal pockets. Gradually, they attack the periodontium which supports teeth. Gums thin out and retract and, once the periodontal ligament and alveolar bone are affected, teeth begin to loosen.
The damage caused by periodontitis is irreversible and tooth loss may occur if the disease is left untreated.
Symptoms
- Tooth sensitivity
- Gingival recession
- Abscesses
- Loose teeth
- Loss of teeth
Treatment
Because of its worrisome consequences, periodontitis should be addressed quickly. The dentist will assess the severity of the situation and develop a suitable treatment plan, which will include:
- Tartar removal
- Deep cleaning of periodontal pockets to eliminate bacteria
- Root planing to remove bacteria stuck on roots
- Antibiotics, if needed
- Reshaping of gums, if needed (gingivoplasty)
- Bone graft, if needed
Periodontal disease is insidious and it can have very detrimental consequences if it isn’t diagnosed and treated in time. Meticulous oral hygiene and regular dental check-ups are essential to preventing it.
Read the article on periodontal disease and general health
Gum grafts
What is a gum graft?
A gum graft is a surgical procedure carried out by a periodontist. The purpose of a gum graft is to restore gums around teeth and their roots. It also serves to curtail gingival recession and prevent further loosening of teeth. A gum graft is an effective solution that treats more than just cosmetic problems.
Understanding gingival recession
Gingival recession is a very common problem where gums shrink. As they gradually thin out and recede, the gums no longer provide adequate coverage, exposing dental roots.
This leads to unpleasant sensitivity to hot, cold, sweet or acidic foods. Exposed roots are also more susceptible to cavities. In severe cases, the gums can no longer properly support teeth, which may become loose and even fall out.
Gingival recession also affects your smile. When gums recede, your teeth appear abnormally long. It is important to curtail this problem as soon as possible because mild cases are much easier to treat.
Symptoms :
- Tooth sensitivity (heat, contact)
- Visible dental roots
- Cavities on roots
- Loose teeth
- Loss of teeth
Risk factors
Some people are more likely to develop gingival recession than others.
- Naturally thinner gums in some areas
- Dental malpositions
- Excessive, vigorous brushing or improper brushing technique
- Involuntary teeth grinding and gritting (bruxism)
- Inadequate dental restorations
- Orthodontic treatments
- Gum disease, periodontitis
Gingival recession is irreversible. To restore the gums and curtail further loosening of the teeth, the dentist must perform a gum graft.
There are three (3) types of grafts
Traditional autogenous grafts
The patient is administered anaesthesia and the affected area is prepped to receive the new tissue. A thin layer of conjunctive tissue is removed from the palate. Then, it is carefully placed on the retracted gum and sutured.
To promote healing, a bandage is applied on the grafted area. The palate will then begin regenerating and heal significantly in the next 15 to 21 days. It will take about six months to heal completely.
The graft, which is composed of strong keratinized tissue, provides increased stability to the affected area and protects it from a further gingival recession.
Because the graft comes from the patient, integration and healing are quick. Since the tissue is not rejected, the success rate is excellent. However, the area on the palate where the tissue was removed will remain sensitive for some time. Also, the possible lengths of grafts are limited.
 Allogenic grafts | AlloDerm®
Allogenic grafts | AlloDerm®
Allogenic grafts are an interesting alternative to traditional grafts because the tissue isn’t taken from the patient’s palate. Instead, the AlloDerm graft comes from a human donor. The donated tissue is processed to create a regenerative tissue matrix made of collagen. This type of graft stimulates the self-healing process of the patient’s tissue.
The procedure is the same as with a traditional graft. The graft is sutured to the affected area to restore the gums around the teeth. Once healing is complete, any dental sensitivity will be gone and the gums will be stable again. Since allogenic grafts don’t use tissue from the palate, they are less painful.
Advantages
- No tissue is removed from the palate, eliminating potential complications and pain
- Cosmetically appealing results
- Excellent success rate
Pinhole® Gum Graft
Pinhole® Graft Technic - A breakthrough treatment for gum recession
The Chao Pinhole® Surgical Technique is a minimally invasive option for treating gum recession. Unlike traditional grafting techniques, PST is incision and suture free. All of the tools and techniques used to perform the Chao Pinhole® Surgical Technique were created by Dr. John Chao, and who trained our doctor.
The difference between the pinhole® Graft Technic and a traditional gum graft
Traditional gum recession treatments involve the use of donor tissue or soft tissue grafts in order to rebuild the gumline. This soft tissue would be sutured in place and would join with existing gum tissue as it healed. While this traditional grafting treatment is effective, comparable results with better patient experience can be achieved through the Chao Pinhole® Surgical Technique.
 The procedure
The procedure
During the Chao Pinhole® Surgical Technique, a needle is used to make a small hole in the patient’s existing gum tissue. Through this pinhole, special instruments are used to gently loosen the gum tissue. These tools help expand and slide the gumline to cover the exposed root structure.
There are no grafts, no sutures, and no incisions needed with the Chao Pinhole® Surgical Technique. It simply involves the adjustment of the existing tissue.
The benefits
The benefits of the Chao Pinhole® Surgical Technique are many:
- Less discomfort for the patient after treatment
- Faster recovery for the patient than traditional grafting
- No need for uncomfortable sutures
- No need for scalpels or invasive surgical tools
- No need to take donor tissue from the patient’s palate
- Excellent, natural-looking, long-lasting results
Prevention
Gum disease, which often causes teeth to become loose, can be very insidious as it is painless at first. If it isn’t diagnosed and treated in time, the consequences of gum disease can be very detrimental. Learning how to brush your teeth gently will protect your gums. Regular dental check-ups and professional cleanings will keep them healthy.
Call your dentist if you have sensitive teeth or if some teeth appear longer due to thinner gums.
Extracting wisdom teeth
Those mysterious wisdom teeth !
Wisdom teeth, also called third molars, are the last of your permanent teeth. They come in at the back of the dental arch between the ages of 18 and 21. Their development is slow and often problematic.
Due to lack of space, wisdom teeth can have trouble coming in or positioning themselves properly. All too often, they are too big for the space available.
Why does this happen?
Over time, the human jaw may have gotten smaller as the size of our teeth remained the same. This would explain why so many people lack the space needed for wisdom teeth to come in properly.
The evolution of our diet toward softer foods means our teeth don’t wear out as much. In the past, wear and tear may have made our teeth smaller, which would have left sufficient space in the dental arch to accommodate wisdom teeth.
An improved diet and better oral hygiene mean that we may lose fewer teeth than our ancestors. Our teeth, therefore, stay in place longer and fill all the available space in our mouth.
Unpredictable teeth...
It can be hard to predict how and when wisdom teeth will come in. They may grow in the wrong direction, come in partially (semi-impacted) or not at all (impacted).
1 | Wisdom teeth growing in the wrong direction
When a wisdom tooth grows in the wrong direction, it puts pressure on the adjoining molar and causes other teeth to overlap or become misaligned.
And, if the wisdom tooth comes into contact with the root of an adjacent molar, it can cause that root to be reabsorbed. Over time, the root will disappear until the tooth becomes weakened or eventually falls out.
2 | Partially erupted wisdom teeth
Sometimes a wisdom tooth only comes out partially, leaving part of the tooth under the gum. This can cause an infection since bacteria tend to penetrate the tissue. Pain, fever and complications, like abscesses or cysts, may occur. A semi-impacted wisdom tooth has to be tended to quickly and often requires an extraction.
3 | Impacted wisdom teeth
Impacted wisdom teeth don’t come in at all. Even though the tooth is mostly formed, it remains under the gum. Nine out of ten people will have at least one impacted wisdom tooth. Sometimes this can cause problems and sometimes it has no consequences whatsoever.
4 | No wisdom teeth (agenesis)
A complete lack of one or several wisdom teeth is also a common occurrence. Wisdom teeth are the most prone to agenesis. In most cases, this doesn’t cause a problem, unless the wisdom tooth on the opposite dental arch comes in. If a wisdom tooth does not have an opposing tooth to rest on during occlusion, it can become loose and may sometimes need to be extracted.
Oral health problems caused by wisdom teeth
- Cavities
- Pain
- Abscesses and cysts
- Gum infections where the tooth has partially erupted
- Deterioration of adjoining teeth
- Overlapping teeth on the dental arch
Extracting wisdom teeth
To avoid complications, it’s sometimes best to remove wisdom teeth. By regularly monitoring their development, the dentist can make sure they come in properly and that the space available is sufficient. X-rays will show what is happening under your gums and help the dentist determine if the teeth need to be removed before they cause problems.
Wisdom teeth are harder to extract than other teeth. Because they are located at the very back of the dental arch and are often impacted in the gum, it is a delicate surgical procedure. A complete exam of your mouth and an assessment of your overall health are needed before an extraction can be performed.
Surgery can be done using local anesthesia, although general anesthesia is sometimes recommended.

Mouthguards
Do you play a team sport or enjoy high-impact recreational activities? Make sure you protect one of your best assets-your smile! Invest in a high-quality mouthguard to minimize injuries to your mouth and teeth.
Made of flexible material, a mouthguard protects your teeth and mouth when playing sports. There are many types of protectors available, but they don’t all offer the same level of protection.

Protecting your teeth is important!
Keeping your teeth and mouth injury-free is just as important as good oral health. Along with regular check-ups and cleanings, a mouthguard can help you maintain a great-looking smile.
A mouthguard protects more than just your teeth. It protects your jaw, temporomandibular joints, tongue and the soft tissues in your mouth. Using a mouthguard won’t prevent 100% of all injuries, but it can certainly help reduce their occurrence and severity.
Because most mouth injuries happen to youngsters, Health Canada1 recommends the use of mouthguards when boxing or playing football, hockey or rugby. A mouthguard should also be considered for basketball, soccer, skiing, inline staking and mountain biking.
Some stats
- Between 13% and 39% of injuries to teeth occur when practicing a sport
- According to the Quebec Order of Dentists (ODQ), approximately 200,000 serious
accidents could be prevented annually with mouthguards - Every year in the United States, approximately 400,000 youngsters suffer concussions
- According to the National Youth Safety Foundation, 3 million teeth are lost each year
while practicing sports in the United States - According to the American Association of Orthodontists, over 67% of parents don’t encourage their children to wear a mouthguard when practicing high-impact sports
Types of mouthguards
Stock mouthguards
This type of mouthguard is a low-cost option that’s available in pharmacies and sporting goods stores. However, stock mouthguards aren’t adapted to your teeth and offer very little protection. In fact, the injury rate while wearing a stock mouthguard device is just as high as not wearing any. And, this device makes it difficult to breathe and speak properly.
Boil-and-bite mouthguards
This type of protector adapts better to your teeth than a stock mouthguard, but still doesn’t offer maximum protection. You must place it in boiling water to soften it and then bite into it so that it takes the shape of your teeth. However, it is not very stable as the thickness of the material varies.
Custom-made mouthguards
This type of device is your best option for practicing sports. Even though custom mouthguards are more expensive, they fit your teeth much better. Since your dentist uses impressions of your teeth to make your custom device, it will be significantly more comfortable and stable, while offering additional protection in some areas.
You can also choose the colour of your mouthguard or even add a logo. It can be adjusted to your orthodontic devices and it won’t impact breathing or speaking.
Important
Custom-made mouthguards are very easy to maintain. Simply rinse with cold water or mouthwash before and after each use, and air dry. Avoid exposing the device to hot temperatures and have it checked by your dentist during your regular check-ups.
Ask your dentist today about a custom-made mouthguard. And, if you sustain an injury to your mouth, see your dentist right away. By taking action quickly, you can avoid major
consequences to your dental health and your smile!
Protège-dent pour les sport — lien vers le site du Gouvernement du Canada
Sedation with nitrous oxide
Despite all the progress made in the field of dental medicine with respect to analgesics and dental techniques, “fear of the dentist” is still very common. For some anxious patients, the idea of going to the dentist is a source of stress and fear. In some cases, this fear prevents them from getting the dental care they need. This is why it is important to take this situation seriously.
Since 2001, an alternative, conscious sedation method has been offered. Nitrous oxide is inhaled, enabling patients to relax while remaining awake. By foregoing other traditional sedation methods, such as general anesthesia, patients don’t have to deal with contraindications and side effects.
What is nitrous oxide?
Nitrous oxide helps patients feel better by eliminating their anxiety. The gas helps patients relax by diminishing anxiety and reactions to painful stimuli, without putting them to sleep. It even affects the perception of time, making patients feel like the procedure went by much faster.

Advantages
- Simple to administer: Patients breathe into a nasal mask. No injections are required.
- Patients stay awake during the entire procedure. They are able to cooperate, answer questions and let the dentist know how they’re feeling.
- A patient’s breathing is unaffected during the entire sedation, making this method very safe.
- The gas acts quickly, in about three to five minutes.
- Once the procedure is finished, oxygen is administered to the patient, immediately neutralizing the effects of the nitrous oxide. In five minutes, the product is completely eliminated from the lungs and no traces of it are left in the body.
- Patients can go back to their normal physical or intellectual activities right away.
- Nitrous oxide can be used on children as young as six.
Benefits
Nitrous oxide (laughing gas) helps patients feel more comfortable, in addition to making the dentist and the rest of the team’s work easier. This sedation method increases patient
safety during more delicate procedures and therefore improves their success rate.
For patients who are afraid of going to the dentist, nitrous oxide is a great option. When anxiety is lessened, it’s easier to see a dentist on a regular basis or as soon as there is a problem. Consequently, treatments are less invasive and the patient experience is more positive, ensuring better oral health in the long run.
Contact us today to find out more about nitrous oxide.
Sleep apnea and snoring
Good quality sleep is essential for a healthy life. It allows us to recover physically, but also benefits the brain, which takes advantage of the night to consolidate its achievements.
Sometimes, rest is disrupted by a disorder called obstructive sleep apnea (OSA). This condition involves repetitive and involuntary suspension of breathing. At every stop, carbon dioxide cannot be expelled, while air and oxygen cannot get to the lungs. To "force" breathing, the brain sends an alarm signal, which causes a wake-up or micro-awakening. A chronic apneic can stop ventilating up to 10 times per hour!
At the Dr. Susan Biner Dental Clinic, we can make mandibular advancement device to control sleep apnea (and / or snoring).
Who has sleep apnea?
According to the Quebec Lung Association, more than one in four adults suffer from sleep apnea. But it is as much men, women as children who are affected. A survey published in 2009 indicated that only 3% of the population over the age of 18 had been diagnosed. However, 26% of undiagnosed adults had symptoms and risk factors related to the disease. So, if in doubt, it is best to see a doctor. The latter will be able to provide the necessary follow-up to offer appropriate treatment to minimize health risks.
Certain conditions can predispose to this disorder:
- Congenital causes (large tonsils, malocclusion, narrow arches)
- Heredity (several cases in the family)
- Taking certain medications
- Smoking
- Consumption of alcohol before bedtime
- Overweight
Signs and symptoms to look out for
The most common nocturnal symptoms are:
- Snoring
- Restless sleep
- Perspiration
- Micro-alarms
- Frequent urge to urinate
- Insomnia
In the short term, the apneic person may feel the effects of an uncomfortable night's sleep upon awakening and sometimes throughout the day:
- Headache
- Fatigue and excessive drowsiness
- Loss of concentration
- Blackout
- Irritability
- Decreased libido or sexual impotence
Due to the cognitive inhibition it causes, sleep apnea can negatively impact performance at work or school. Loss of vigilance also puts you at greater risk of being the victim of an accident at work or on the road.
In the long term, this sleep disorder predisposes to various serious illnesses: hypertension, stroke, heart problems, diabetes, cancer, obesity, premature labor, epilepsy, loss of libido, depression, anxiety and even sudden death.
In the long term, this sleep disorder predisposes to various serious illnesses: hypertension, stroke, heart problems and even depression. But the reverse is also true as these and other medical conditions such as diabetes, paralysis, hypotyroidism, cancer or high cholesterol can in turn lead to apnea.
Solutions to stop sleep apnea
Several solutions exist to improve his lot. The first is to adopt healthy sleep hygiene, including limiting the consumption of tobacco, alcohol and sedatives before bed.
Since obesity is a risk factor, it is best to consider weight loss.
Finally, after a complete assessment of your risk of apnea and a sleep test, a pulmonologist will be able to tell you whether a mandibular advancement device or CPAP (continuous positive pressure device) will be appropriate for your condition.
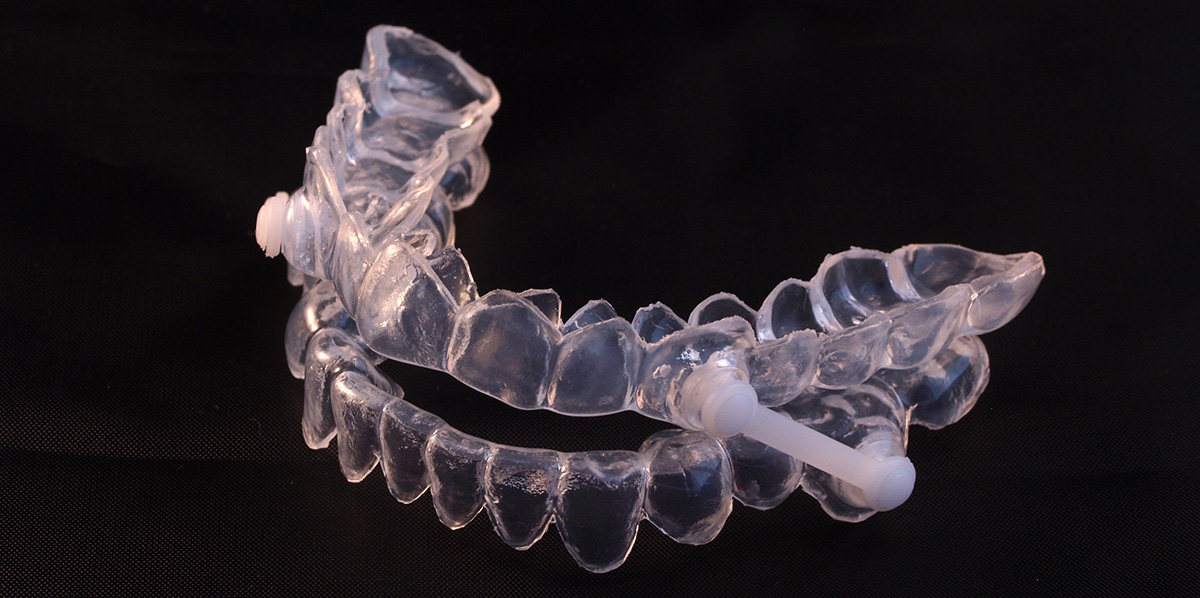
If your apnea is severe then the treatment of choice is CPAP. If your apnea is mild to moderate or if you cannot wear the CPAP, you will be recommended a mandibular advancement device, designed by the dentist. There are also surgeries to correct anatomical problems (large tonsils, uvula, adenoids, etc.).
It is very important to have a diagnosis from a sleep doctor (often a pulmonologist).
The Dr. Susan Biner Dental Clinic will be happy to coordinate for you all the necessary steps to obtain a thorough examination, a sleep test as well as the pulmonologist's diagnosis. This will allow her to identify if you have this syndrome and if you are a candidate for mandibular advancement device or CPAP.
Above all, do not neglect a doubt. If you snore, are irritable and distracted, or never rested, tell your doctor. Studies show, sleep apnea:
- Affects people of all ages
- Reduces life expectancy
- Promotes the development of serious medical conditions
An easy test can shed some light and maybe a simple mandibular advancement device could make a difference.
If I snore, do I have apnea?
FALSE. A snorer is not always apneic. Snoring is caused by the air vibrating the soft tissues in the throat (soft palate, tonsils, uvula).
However, it can be symptomatic of a more serious disorder, such as OSA. If you are concerned, do not hesitate to come and consult us.
Consult the complete information by clicking here.

Jaw disorders
What is the TMJ?
The temporomandibular joint (TMJ) connects the lower jaw to the skull’s temporal bone. By placing your fingers on each side of your face, in front of your ears, you’ll feel the joint move when you open and close your mouth. The TMJ enables many ranges of motion: back and forth, opening and closing, and side-to-side. It’s a sensitive junction through which many important structures pass, including nerves, muscles, blood vessels, ligaments, and tendons. Without a doubt, the TMJ is one of the human body’s most complex joints.
What is a jaw disorder?
When all of the TMJ’s components are working properly, you can chew, speak and yawn without any difficulty. But when the two joints are misaligned, or the protective articular disk has shifted or been injured, the joint can’t function properly. This is known as a temporomandibular disorder (TMD).
TMDs affect your ability to chew. They can be muscular, articular or arthritic (inflammatory) in nature. Approximately 50% of the general public will suffer from a TMD during their lifetime, but only 1 out 10 people will see a dentist about it.

Symptoms of a TMD
The symptoms of a jaw disorder often include painful stiffness and blocking, as well as :
- Pain in front of ears
- Pain and discomfort that spreads over the face, jaw, neck and/or shoulders
- Difficulty opening the mouth
- Inability or difficulty closing teeth together
- Headaches and migraines
- Difficulty chewing or speaking
- Sudden occlusion changes
- Joint cracking or grinding
While these symptoms may completely disappear with time, they often become chronic, causing lasting pain.
Causes of TMDs
TMDs have many causes. In fact, they’re due to a complex combination of several factors, including:
Injury
A car accident or a head injury sustained while playing sports may have led to a jaw fracture or damage to the articular disk.
Bruxism
Bruxism often occurs at night. A subconscious contraction of the jaw causes excessive grinding or gritting of the teeth. The pressure exerted on teeth is several times greater than during chewing, leading to worn, fractured or loose teeth.
Stress
Stress and anxiety can affect people in different ways. They can cause increased tension in the back, shoulders and jaw. By repeatedly gritting one’s teeth, jaw muscles become stiff and tired. Compulsive gum chewing and nail-biting are other habits to avoid.
Malocclusion | poor contact between teeth
Malocclusion occurs if the top and bottom teeth aren’t properly supported when the jaw is closed or during chewing. It is caused by :
- Dental overlapping
- Excessive or insufficient overlay
- Jaw misalignment
- Missing or excessive teeth
- Imbalance between top and bottom jaw
- An accident
The following factors can also lead to a TMD :
- Arthritis
- Poor posture
- Lack of sleep
- Sleep apnea (snoring)
Possible treatments
Approximately 80% of TMDs are temporary and symptoms disappear within six months, without any treatment needed. It’s important to let the jaw relax and to reduce swelling. We recommend :
- Taking mild painkillers
- Avoiding hard foods and intense chewing (gum)
- Avoiding opening your mouth too wide
When a TMD is caused by malocclusion, an orthodontic treatment may be needed. For bruxism, a biteplate at night can reduce friction and help position your jaws. Also, finding ways to deal with stress or avoid it altogether will go a long way in helping you relax.
Treating a TMD first requires a careful, multifactor assessment by a dentist. Then the dentist will develop an intervention plan to address your needs so that you can achieve optimal dental well- being.
Additional
information
Tools to simplify life
Patient Section
In order to serve you better, we have put together a wealth of information, useful documents and informative texts in this section. You can also make an appointment directly online.
Take the time to consult it, but know that we are always available and happy to answer all your questions!
The start of good habits
Children's Corner
We have made additional information about your children's health and oral hygiene available to you. There you will find some tips to start the hygiene process on a good basis and teach them good habits.
Take the time to consult it, but know that we are always available and happy to answer all your questions!
For your well-being
Post-surgery Advice
In order to make you feel better prepared after dental surgery, we have put in some documentation as a guide and postoperative advice. We strongly suggest that you refer to it to avoid any complications or unfortunate situations.
Take the time to read it, but know that we are always available and happy to answer all your questions!
Questions and/or comments?
Don't hesitate to contact us
We will always be happy to answer all your questions and provide you with more information about our products and services. We also appreciate reading your comments and opinions so write to us.


